Impact of socioeconomic status on initial clinical presentation to a memory disorders clinic.
Impact of socioeconomic status on initial clinical presentation to a memory disorders clinic.
Qian W, Schweizer TA, Fischer CE.
Keenan Research Centre of the Li Ka Shing Knowledge Institute at St. Michael’s Hospital, Toronto, Canada.
ABSTRACT:
BACKGROUND: Dementia affects 15% of Canadians 65 and older, and the prevalence is expected to double over the next two decades. Low socioeconomic status (SES) can increase the risk of Alzheimer’s disease (AD) and the precursor mild cognitive impairment (MCI), but it is unknown what the relationship of SES is on initial clinical presentation to a memory disorders clinic.
METHODS: Data from 127 AD and 135 MCI patients who presented to our Memory Disorders Clinic from 2004 to 2013 were analyzed retrospectively. We examined the relationship between SES (measured using Hollingshead two-factor index) and (1) diagnosis of either AD or MCI; (2) age when first presented to clinic; (3) objective cognitive tests to indicate clinical severity; and (4) the use of cognitive enhancers, medication for treating mild-to-moderate AD patients.
RESULTS: AD patients had lower SES than MCI patients (p < 0.001, r = 0.232). Lower SES was associated with a greater age at initial time of diagnosis (χ2 = 11.5, p = 0.001). In MCI patients, higher SES individuals outperformed lower SES individuals on the BNA after correcting for the effect of age (p = 0.004). Lower SES was also associated with decreased use of cognitive enhancers in AD patients (p < 0.001, r = 0.842).
CONCLUSION: Individuals with lower SES come into memory clinic later when the disease has progressed to dementia, while higher SES individuals present earlier when the disease is still in its MCI stage. There were more higher SES individuals who presented to our memory clinic. Higher SES is associated with better cognitive functioning and increased use of cognitive enhancers. The health policy implication is that we need to better engage economically disadvantaged individuals, perhaps at the primary care level.
PMID: 24331159
SUPPLEMENT:
Alzheimer’s disease (AD) is the most common type of dementia and is associated with significant cognitive and functional decline. Mild cognitive impairment (MCI) is a brain syndrome often considered to be the transition stage between normal aging and Alzheimer’s disease. While there is a genetic component to AD, there are many environmental factors that can influence the onset and progression of the disease. Socioeconomic status (SES), defined by some a measure of educational level combined with occupational attainment, is a factor that has been shown to reduce the risk of AD and dementia, although its effects on MCI have not been as extensively investigated. While it appears that the diseases themselves are more common among low SES population, it is not known how SES impacts medical referral to a memory disorders clinic. Initial presentation is of importance because earlier detection and diagnosis of the disease can lead to more effective treatment with cognitive enhancers, medication for treating mild-to-moderate AD patients.
Our study looked at how SES can influence the initial presentation to the Memory Disorders Clinic at St. Michael’s Hospital located in the urban setting of Toronto, Canada (Figure 1). We hypothesized that lower SES would negatively impact medical outcome by delaying the detection and diagnosis of AD. Patients seen at the clinic, which subserves a population with a wide range of SES, are referred from their family physicians. SES was measured using Hollingshead two-factor index, which combines educational and occupational attainments. The index ranges from 11-77 and is negatively correlated with observed SES. Healthcare is fully funded by the provincial government through the Ontario HeOur results supported our hypothesis. We found that patients with AD at presentation to our memory clinic had lower SES than patients with MCI (Figure 2), and that lower SES patients present to clinic at an older age; about 4 years older. In addition, within patients with MCI, lower SES was associated with greater disease severity as measured by extensive cognitive tests. Next, we investigated the use of cognitive enhancers between high and low SES patients with AD and found that lower SES was associated with reduced use of cognitive enhancers (Figure 3).
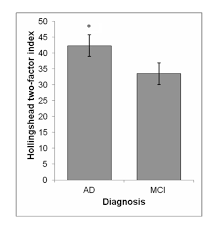
Mean Hollingshead index scores between Alzheimer’s disease (AD) and Mild Cognitive Impairment (MCI) patients. Note: Hollingshead index is inversely related to socioeconomic status.
These results suggest that higher SES may lead to earlier disease detection and referral to memory clinics so doctors can catch the disease while it is still in its MCI stage. In contrast, individuals with lower SES delay medical attention until the disease has already progressed to dementia. There could be several factors that could explain these findings. It has been documented that low SES patients tend to experience more co-morbidities such as hypertension and diabetes, so in light of their physical health issues cognitive impairments may take a back seat. High SES individuals may also be better read and are more knowledgeable on the symptoms of AD and consequently seek medical attention when they recognize the signs. Another possibility is that it may be easier to detect cognitive decline in those with a higher cognitive baseline, as in the case in those with higher education and occupations that may be more cognitively demanding. Lastly, SES could contribute to “cognitive reserve”, which buffers the brain against disease onset through increased brain stimulation, although we cannot know this without further brain imaging.
Regardless of the specific reason, our findings suggest that higher SES is associated with better outcome through earlier disease detection and diagnosis. Timely diagnosis of AD, like many other illnesses, proves to be valuable for a number of reasons. Early identification can allow for more time for the patient and their family to make decisions concerning disease management and forward planning as well as allow treatment for the modifiable aspects of the dementia. Cognitive enhancers, medication for treating dementia, are most effective if given in the mild-to-moderate stages of the disease. We found that AD patients with lower SES had reduced use of cognitive enhancers, either because the treatment was refused, or, more likely, they were not candidates because they were too advanced in their disease progression to benefit from cognitive enhancers.
In addition to delayed presentation to memory clinics, we found that lower SES patients are less likely to come in at all as there was an over-representation of higher SES individuals who attended our memory clinic. As such, the predicament is that while dementia and AD are more prevalent among the low SES population, these individuals are less likely to seek medical attention, and when they do, they come at a more advanced disease stage and are thus less able to benefit from treatment. Despite being in a country with universal healthcare that eliminated the barrier of cost of medication and medical care, our study indicate that disparities in economic wealth and education can still influence medical outcome; the economically disadvantaged still face inequalities when it comes to the diagnosis and treatment of AD.
Our findings call for a change in health policy to better engage patients with low SES, perhaps at the primary care level. Primary care physicians should be more proactive in screening these economically disadvantaged patients as they are less likely to present to memory clinics. This would enable these patients to be identified and treated earlier, resulting in improved treatment outcomes.
Mohamed E. Salem, MD, Levine Cancer Institute, Charlotte, NC
 Euro
Euro
 US Dollar
US Dollar
