Iron status of pregnant Indian women from an area of active iron supplementation.
Menon KC, Ferguson EL, Thomson CD, Gray AR, Zodpey S, Saraf A, Das PK, Pandav CS, Skeaff SA.
Department of Human Nutrition, University of Otago, Dunedin, New Zealand
Abstract
OBJECTIVE: The aim of this study was to investigate the iron status of pregnant tribal women from Ramtek, Nagpur, Maharashtra, India using a combination of indices.
METHODS: A community-based observational study was conducted to assess iron status using a convenience sample of pregnant Indian tribal women from Ramtek. Pregnant women were recruited at 13 to 22 wk gestation (first visit; n = 211) and followed to 29 to 42 wk gestation (second visit; n = 177) of pregnancy. Sociodemographic and anthropometric data; iron supplement intake; and blood samples for estimating hemoglobin (Hb), serum ferritin (SF), soluble transferrin receptor (sTfR), and C-reactive protein (CRP) were obtained.
RESULTS: The mean (SD) Hb concentration at recruitment was 106 (15) g/L and 106 (14) g/L at the second visit; 41% of the women at recruitment and 55% at second visit were anemic (14% higher, P < 0.001). No women at recruitment and 3.7% at second visit had SF concentration < 15 ng/mL; and 3.3% at recruitment and 3.9% at the second visit had sTfR > 4.4 ng/mL (0.6% higher, P = 0.179). Almost 62% and 71% of pregnant women used iron supplements at both visits, respectively. Iron supplement intake > 7 d in the preceding month improved the Hb concentration by 3.23 g/L and reduced sTfR concentration by 13%; women who were breastfeeding at the time of recruitment had 11% higher SF concentration.
CONCLUSIONS: The iron indices suggest that pregnant tribal women of central India, although anemic, had good iron status. Use of iron supplements > 7 d in the preceding month improved iron status; however, non-iron-deficiency anemia persisted in this group. Copyright © 2014 Elsevier Inc. All rights reserved.
KEYWORDS: Anemia; Dietary supplements; Iron deficiency anemia; Iron status; Pregnant women
PMID: 24484679
Supplement:
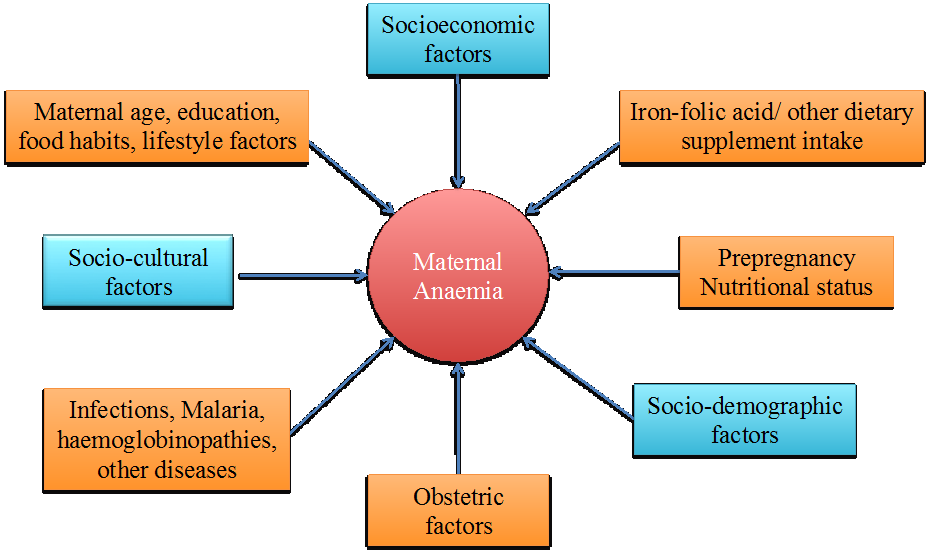
Maternal anaemia is a critical public health issue in India. Many efforts are underway to combat the high prevalence of anaemia in pregnant Indian women. In India, multiple supplementation programmes are implemented to address this issue including free iron-folic acid supplementation, distribution of double fortified salt with iron and iodine in selected districts, and fortification of foods. All the above pre-emptive programmes assume anaemia is primarily due to an inadequate dietary intake of iron, from poorly bioavailable cereal-pulse-based vegetarian diets. However, anaemia may occur for reasons other than iron deficiency including repeated infections, malaria, concurrent micronutrient deficiencies of vitamin A, vitamin C, copper, folate, riboflavin, vitamin B12 and vitamin B6, and haemoglobinopathies such as thalassaemia and sickle cell anaemia that influence the synthesis of red blood cells.
A first survey was conducted in 2007 of nonpregnant tribal and rural Indian women to investigate their micronutrient status and we observed that pregnant women in this area were actively supplemented with iron-folic acid and other micronutrient supplements (1). The term “actively” refers to a process used to distribute supplements through simultaneously through multiple channels (i.e. health centres and health professionals), in contrast to more passive or limited distribution of such supplements. The paucity of data on the iron status of actively supplemented pregnant Indian women and a high prevalence of anaemia in nonpregnant women warranted further investigation. This paper is reporting the results of the second survey, conducted in 2008 in the same region, and evaluated the iron status of pregnant women using multiparametric indices as recommended by the World Health Organization/Centers for Disease Control Prevention (2). We used a combination of indices such as haemoglobin (a measure of functional iron deficiency), serum ferritin (a measure of storage iron deficiency) and soluble transferrin receptors (a measure of tissue iron deficiency) along with a marker for infection, C-reactive protein. The pregnant women were tested for the sickle cell trait. Information on the use of iron containing supplements was collected at two time points, the first visit when women were in their second trimester and the second visit when women were in their third trimester. We hypothesized that women who used iron supplements would have better iron status and a lower prevalence of anaemia.
In contrast to other studies, we observed that pregnant Indian women who used iron-containing supplements >7 days in the preceding month had good iron status and relatively lower prevalence of anaemia, despite the intermittent use of these iron-containing supplements. The use of iron-containing supplements for >7 days in the preceding month also predicted higher haemoglobin, higher serum ferritin, and lower soluble transferrin receptor concentrations indicating good iron status in these pregnant women.
The findings from the present study are particularly relevant for pregnant women from developing countries, public health workers, health professionals and policy makers. Firstly, the study indicated that free iron-folic acid supplements in conjunction with the other micronutrient supplementation improved the indicators of iron status in pregnant Indian women. Secondly, an overwhelming proportion of pregnant women consumed one to six iron containing supplements that was likely partly responsible for their improved iron status. Thirdly, pregnant women still nursing a child from a previous pregnancy had better body iron stores than pregnant women who were pregnant for the first time and who were not nursing another child. Finally, although the supplementation programme benefited the women and improved their iron status, anaemia persisted in more than half of these women.
Our study alludes to the intricate multidimensional nature of anaemia and underlines the fact that dietary supplementation of pregnant Indian women improves their iron status. However, dietary supplementation is not a panacea for anaemia. Merely supplementing women with little effort to determine the underlying causes of anaemia including relevant hematological and biochemical evaluation is unlikely to combat the high prevalence of anaemia that currently exists in pregnant Indian women. Also, free iron-folic acid supplementation with inadequate supervision may prove to be detrimental to the health and wellbeing of these women, as excessive iron intakes might subsequently adversely influence pregnancy and infant outcomes. In addition, the myriad of socioeconomic, cultural, dietary and health determinants of anaemia need to be identified and addressed simultaneously with supplementation to ameliorate the issue of anaemia in pregnant Indian women.
Acknowledgements:
The study was supported by a University of Otago Research Grant and the Department of Human Nutrition’s Performance Based Research Fund.
Contact:
Associate Professor Sheila Skeaff and Dr Kavitha Menon, PhD
Department of Human Nutrition,
University of Otago, Dunedin,
New Zealand 9054
Tel: +643 479 5763; Fax: +643 479 7958.
E-mail address: Sheila.skeaff@otago.ac.nz
kavitha.menon@otago.ac.nz
References
- Menon KC, Skeaff SA, Thomson CD, Gray AR, Ferguson EL, Zodpey S, Saraf A, Das PK, Toteja GS, Pandav CS. 2011 Concurrent micronutrient deficiencies are prevalent in nonpregnant rural and tribal women from central India. Nutr. 27(4): 496–502
- WHO/CDC (World Health Organization/Centers for Disease Control and Prevention). 2005 Assessment of iron status at the population level: report of a joint WHO/CDC technical consultation. Geneva, Switzerland: WHO.
 Euro
Euro
 US Dollar
US Dollar
